Detecting reasons for recurrent deformity in treatment of patients with vitamin D–resistant rickets using diagnostic imaging
Views: 1123
Galina Viktorovna Diachkovaa, Konstantin Igorevich Novikovb,∗, Mohammad Reza Effatparvarc, Elena Aleksandrovna Chistovaa, Konstantin Aleksandrovich Diachkova,
Olga Stepanovna Novikovaa, Anatoly Yakovlevich Korkind, Natalia Gennadyevna Shikhalevae
a X-ray Department, Russian Ilizarov Scientific Centre “Restorative Traumatology and Orthopaedics”, ul.M.Ulianovoy, Kurgan, 640014, Russia
b Trauma and Orthopaedic Department No.18, ul.M.Ulianovoy, Kurgan, 640014, Russia
c Department of Biomedical Engineering, Faculty of Engineering, University of Isfahan, Isfahan, Iran
d Trauma and Orthopaedic Department No.17, Russian Ilizarov Scientific Centre “Restorative Traumatology and Orthopaedics”, Kurgan, Russia
e Trauma and Orthopaedic Department No.13, Russian Ilizarov Scientific Centre “Restorative Traumatology and Orthopaedics”, Kurgan, Russia
A R T I C L E I N F O
Keywords:
Vitamin D-resistant rickets Ilizarov externalfixation Diagnostic imaging
A B S T R A C T
Purpose:To assess age related manifestations of the femur and tibia in patients with vitamin D-resistant rickets (VDR) and explore causes for recurrent deformity using imaging modalities.
Methods:Computed tomography (CT), magnetic resonance imaging (MRI) and dual energy X-ray densitometry (DEXA) were used to assess conditions of long bones of lower limbs in patients with vitamin D-resistant rickets aged from 4 years to 30 years preoperatively and after limb lengthening.
Results:Age related MRIfindings showed specific structure of the femur and tibia in patients with VDR pre- operatively and after operative treatment. Abundant irregular osteoid formed in femoral and tibial physes was shown to reveal complicated nature of bone deformity causing recurrence in patients with VDR at childhood. CT findings allowed us to detect early cortical injury, measure its length with forming Looser’s zones, examine significant differences in density measurements of Looser’s zones preoperatively and after deformity correction using transosseous osteosynthesis.
Conclusion:Recurrent deformity can develop in patients with VDR due to progression of the disease, irregular osteoid deposited in the medial and lateral metaepiphysis, osteoid area measuring over 50% of epiphyseal cross section, insufficient regenerate mineralization, and formation of Looser’s zones.
1. Introduction
Pediatric treatment of post-rickets deformity is rather challenging, requires several stages and lasts for many years.1 VDR (hypopho- sphatemic) is the most frequently encountered form of rickets among metabolic disorders. The prevalence of the disease is 1:20000.2 Patients with rickets-like diseases develop lower limb deformities due to dis- turbed physeal metabolism making diagnosis difficult at childhood.3,4 Thanks to the method of transosseous compression-distraction osteo- synthesis pioneered by G.A.Ilizarov the new practice has initiated a qualitatively new approach and greater possibilities for rickets defor- mity correction.5–7 Application of additional osteogenesis stimulation andfixation techniques in patients with VDR allowed for obtaining new rewarding evidence.8–12 A few publications report errors, complications
and recurrence rate of lower limb deformity but no detailed roentgen- morphological assessment of factors causing recurrent deformity in patients with skeletal metabolic conditions has been reported.1,13 The purpose of our study was to get answers to the questions as follows,
- Are there any age related specific features in osseous structures preoperatively and after lengthening in patients with VDR?
- What are the reasons for recurrent deformity in patients with VDR after surgical treatment?
∗ Corresponding author.
E-mail addresses: irina.saranskih@rncvto.ru (G.V. Diachkova), kinovikov@mail.ru (K.I. Novikov), M.r.effatparvar@outlook.com (M.R. Effatparvar), Ryazarova2008@mail.ru (E.A. Chistova), dka_doc@gmail.com (K.A. Diachkov), Ortopediya17@mail.ru (A.Y. Korkin), Nshihaleva@mail.ru (N.G. Shikhaleva).
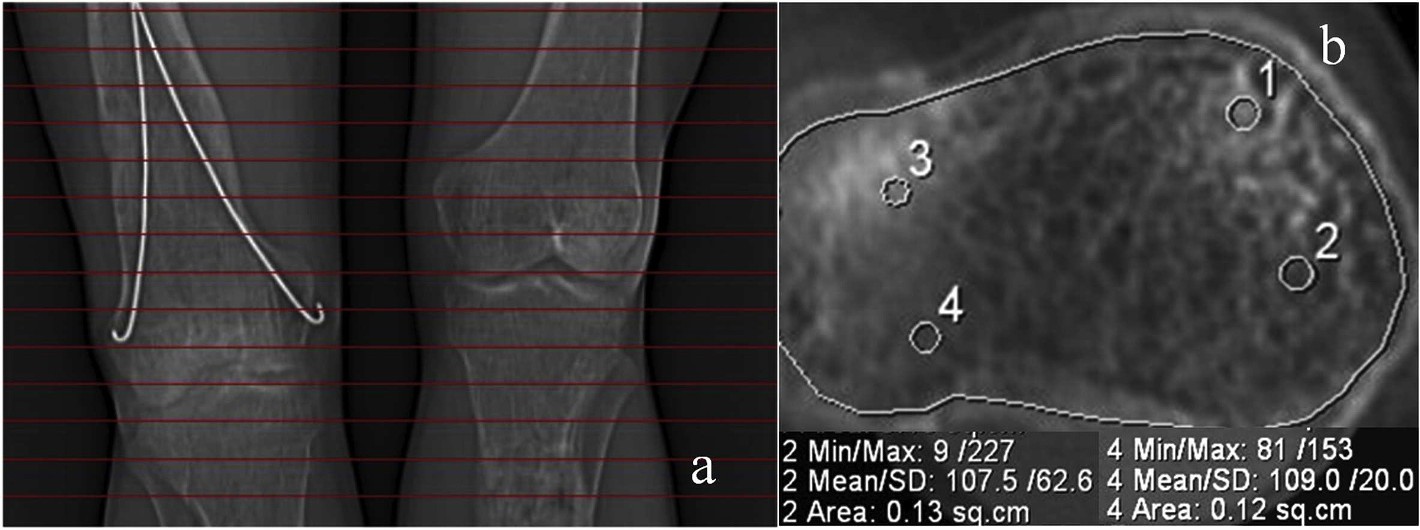
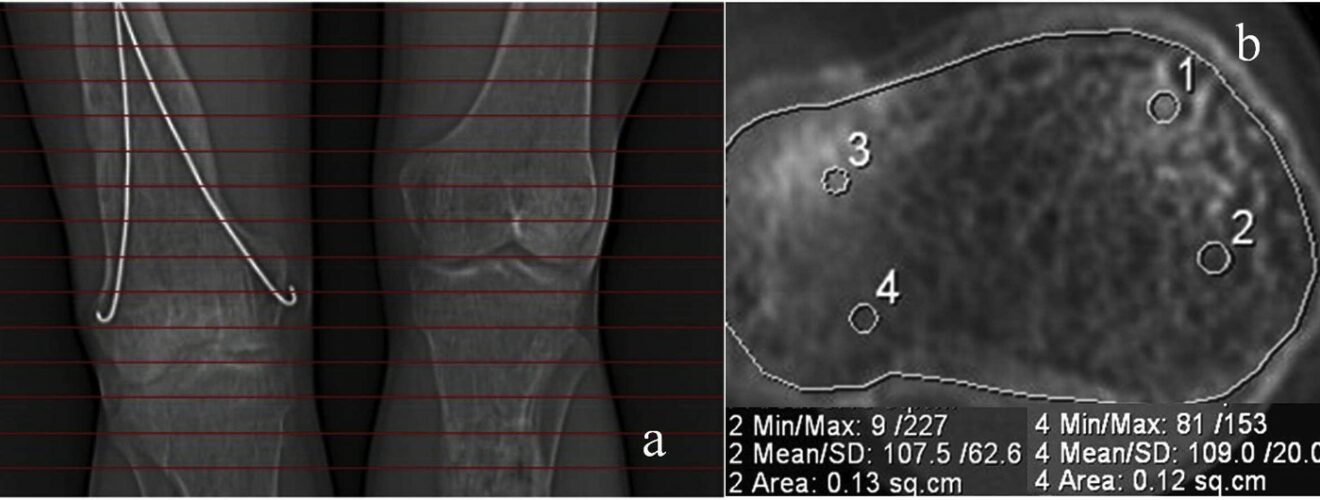
Fig. 1.Total and local bone density measured from cтscans of the knee joints. Topodramm (a), axial plane (b) of the proximal metaphysis of the right tibia in a 21- year-old patient.
Methods
-
- Population
The study included results of treatment and examinations of 62 patients with VDR (phosphate diabetes) aged from 4 years to 30 years. There were 25 female patients (40%). Patients aged from 11 to 16 years (34%) prevailed in the study group. Eighteen patients (29%) started operative treatment at the age of 4–6 years, 17 patients (27%) at the age of 7–10 years, four patients (6%) were operated on at the age of 16–25 years, and two cases (3%) at the age of 25–30 years. All patients received treatment from 1980 to 2011. All patients were seen and di- agnosed by geneticist. Treatment of patients included both conservative and operative techniques. Conservative treatment was tailored and depended on severity, course of the disease, and the patient’s age and included conventional vitamin D therapy or oxidevitum as an alter- native, calcium, phosphorus, vitamins A, C, E and group B medica- tions.14 Phosphorus buffer systems have been recently used. Surgical correction was produced in stable clinical and laboratory remission. Clinical examination showed deficient height, pains in lower limb bones.
-
- Methods of treatment
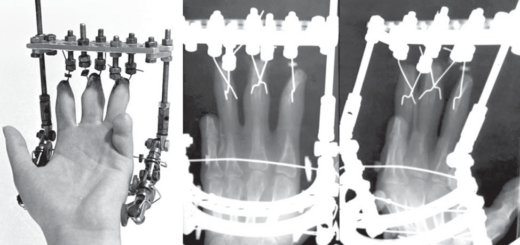
All patients were treated with transosseous osteosynthesis using the Ilizarov externalfixation only or in combination with intramedullary hydroxyapatite coated wires.15 A choice for surgical correction tech- niques and beginning of the treatment was exercised with regard to the patient’s age, severity, type and level of a deformity, number of in- volved segments. Comprehensive metabolic panel and urine test. Pa- tient’s age was disregarded in severe bone deformity to prevent further changes in the joints and spinal column. However, recent evidence suggests that other factors of bone origin participate in maintaining phosphorus homeostasis, includingfibroblast growth factor 23, matrix extracellular phosphoglycoprotein, and frizzled-related protein 4. These factors are collectively known as phosphatonins.16 Calculations using center of rotation of angulation offered by D.Paley (2002) were applied when planning a surgical intervention to identify a level, plane of os- teotomy and number of osteotomies.6 The technique of transosseous osteosynthesis with Ilizarov externalfixation combined with in- tramedullary hydroxyapatite coated wires was used for majority of the patients.
Thirty patients underwent gradual deformity correction and devel- oped distractional regenerate bone and acute deformity correction was produced in 32 cases.
-
- Diagnostic imaging
Computed tomography (CT), magnetic resonance imaging (MRI) and dual energy X-ray densitometry (DEXA) were used for assessment
of 62 patients with VDR preoperatively and at a long-term follow-up. CT scanning was performed using CT Somatom AR.HP (Siemens, Erlangen, Germany). MRI assessment was performed using a 1.5-T MRI Magnetom Symphony Maestro Class unit (Siemens, Erlangen, Germany). Mineral density (MD) of the distractional regenerate bone was measured using Lunar DPX NT bone densitometer (General Electric, USA).
Results
- Preoperative CTfindings showed irregular trabecular patterns and greater distance between them in the femur and tibia metaepiphyses of 80% of the patients with VDR. Absence of typical cancellous bone pattern, thin cortex and lower density values in epiphyses and medial femur and tibia metadiaphyses were observed in patients aged 13–16 years. Bone density in the proximal tibial epiphysis showed greater values in all patients with D-resistant rickets aged 17 years–23 years as compared to the one in the distal femoral epi- physes.
Preoperative assessment of bone structure in patients with VDR aged 24 years–40 years showed areas of heterogeneous cancellous bone in both epiphyses and metaphyses. Bone structure of tibial and femoral metaepiphyses in patients with VDR aged 11 years–16 years appeared as scattered bone trabeculae medially and irregular sclerotic areas at one-to-two-year follow-ups. Patients aged 18 years–23 years showed greater sclerotic changes in the proximal tibial epiphyses and less changes in the distal femoral metaphyses at one-to-three year follow-up which is showed in Fig. 1.
Minimal bone density measurements were observed in the proximal tibial epiphysis of patients with VDR aged 24 years–30 years and deemed to be associated with extensive cysts at the level.
- Bone regeneration (new bone formation) was shown to delay building periosteal and endosteal “bridges” in patients with VDR who underwent acute deformity correction with the total decrease in bone mineral density. Complete organotypical remodeling oc- curred two to three years later. Application of intramedullary wires was practical for reducing treatment length.
A greater diversity in regenerate bone structure was observed during gradual deformity correction in patients with VDR. Areas offine mesh and coarse trabecular structure with lucent cysts were observed.
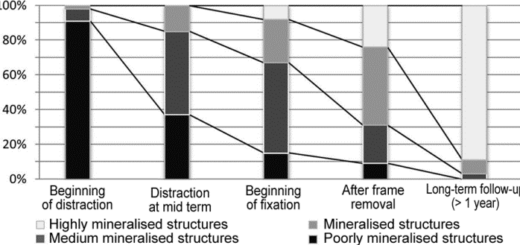
Densitometricfindings showed maximal values of mineral density in the middle part of the femoral regenerate bone of patients with VDR at four-to-five day follow-up. A greater increase in the density was ob- served in the middle part of the femoral and tibial regenerate bone at four-to-six month as compared to distal regenerate portions.
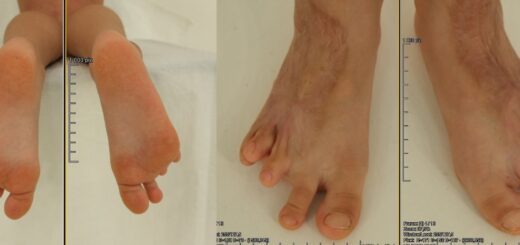
- Preoperative MRI scans of patients with VDR aged tofive years
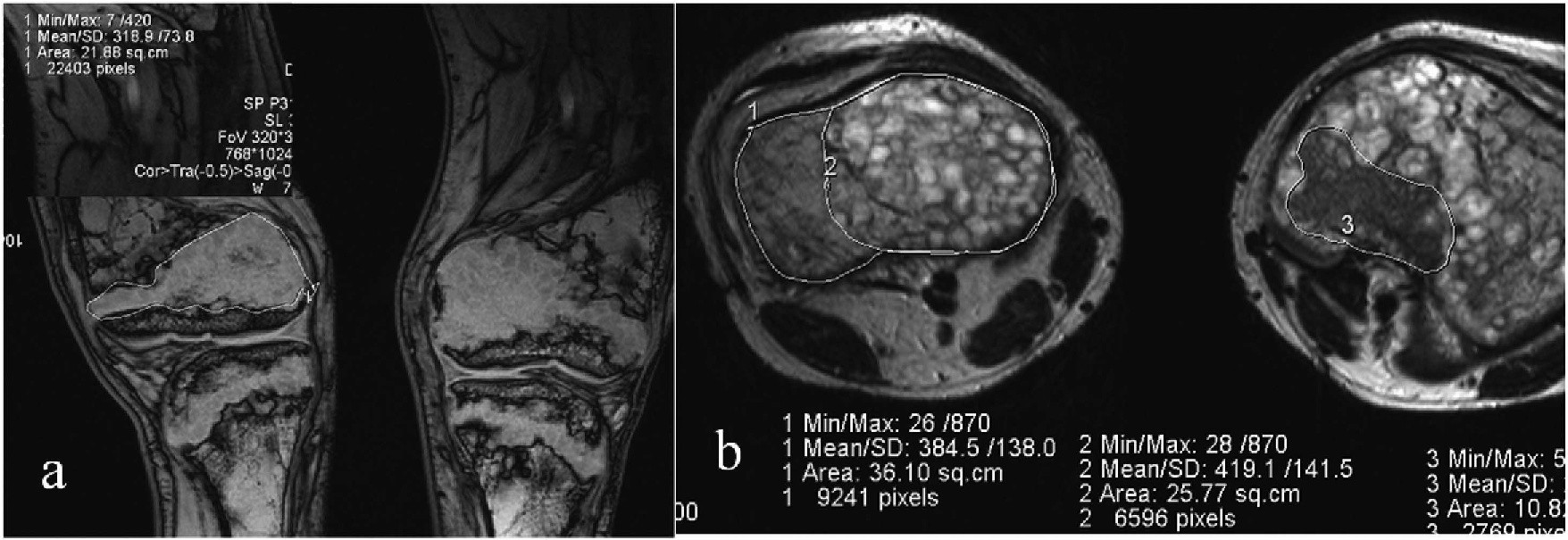
Fig. 2.Osteoid area measured from coronalТ2WI- (a) and axialТ2WI-MRI scans of the knee joints of a 15-year-old patient. With VDR. Measuring osteoid density in coronal and axial planes (b).
showed proliferation of pathologically changed cartilaginous tissue with increased MR-signal onТ1FL2D (FLASH). Patients aged from 9 years to 12 years showed non-mineralized areas (osteoid) at physes extending to femoral and tibial epiphyses and metaphyses revealing irregular, grotesque forms that were well visualized withТ1FL2D FS in the coronal plane preoperatively
MRI scans (Т2TSE) of patients aged from 13 years to 16 years showed a great number of clumpy areas with regular contours and high MR-signal in the femur and tibia epimetaphyses after treatment. To determine an extent of rickets process we suggested calculating a ratio of pathological cartilaginous area (osteoid) and the total epiphyseal, metaphyseal area using MRI scans of the knee joints in Fig. 2.
Round heterogeneous foci of an area measuring to 2.3 ± 0.03сm 2, having obvious wavy contours, and being hyperintensive withТ1FL2D FS,Т2TSE were observed in condyles of patients with D-resistant rickets aged 25 years–30 years after the treatment.
- Changed architectonics of lower limb bones in 17 patients with VDR appeared as pathologically restructured areas (Looser’s zones) ex- tended to the shaft.17 That were addressed with Ilizarov external fixation and intramedullary wires.10–12,17 Looser’s zones were shown to complete after deformity correction. CT scansfirst allowed for detecting specific features of bone structure of the completed Looser’s zones with three-dimensional reconstruction. Thick rolls were visualized in periosteum in the cases with VRT-reconstruction. Looser’s zones were most evident with minimal density measure- ments in patients aged 12 years–16 years.
- A recurrent deformity has been shown to develop in 54 patients with VDR rickets due to:
- Progression of the disease with irregular formation of osteoid zones in the medial and lateral metaepiphysis; increase in os- teoid area of more than 50% of epiphyseal cross section;
- Insufficient mineralization of the regenerate bone in the distal tibia with mineral density of the distractional regenerate bone measuring not more than 750.14 ± 35.70 g/cm2
- Formation of Looser’s zone and bone deformity.
Discussion
Classical radiological rickets manifestations are well known, how- ever, there have been several specific pathomorphological changes re- vealed in the long bones of lower limbs in patients with VDR, and CT, MRI and DEXA that are not routinely used for the condition were em- ployed for detailed evaluation of the femur and tibia metaepiphyses.18 Radiologicalfindings allowed us to pinpoint age-related radiological dynamics in the femoral and tibial physis in patients with VDR. Scat- tered abundant osteoid deposited in femoral and tibial metaepiphysis
served a reason for a complicated deformity in pediatric patients with VDR.19 With greater osteoid deposits that persisted at the age of 14 years–15 years prognosis of classical operative deformity correction was rather problematic. A few publications on MRI assessments of rickets cases described specific features of physeal structure18 however, wefirst performed MRI studies for patients with different types of rickets that allowed for detecting age-related pathomorphological manifestations in the femur and tibia structure preoperatively and at a long-term follow-up.20
CTfindings allowed us to identify an injury to the cortex at an early stage with forming Looser’s zones and its dimensions that was practical for the choice of operative intervention.17 CT and MRI scans have considerably extended the possibilities of morphological assessment of Looser’s zones and their restructuring after the deformity correction.
This is thefirst study of patients with VDR that employed current imaging modalities to assess age related dynamics in pathological changes taking place in the bones of lower limbs to identify risk factors for recurrence following surgical deformity correction. Our sample size has enabled us to detect changes in bone structure of children aged 4 years–15 years that should be considered when planning age and techniques for surgical treatment. In addition to that, we have studied quantitative and qualitative characteristics of Looser’s zones that are also to be considered in treatment of these patients. Thanks to current imaging modalities we revealed causes that could contribute to recur- rence. However, the study does have a number of limitations. First, we had a comparatively small number of adult patients with VDR rickets whose knee bone architectonics was assessed with CT. But these changes were very specific and we can suppose that considerable changes occurring in the femur and tibia metaepiphysis can lead to early deforming arthritis and extensive resorption areas in condyles. Second, not all the patients underwent CT and MRI assessments, how- ever, thefindings have enabled us to identify specific changes in physis and Looser’s zones.
Our study is consistent with previous studies of surgical treatment of patients with different types of VDR that have demonstrated possibi- lities with transosseous osteosynthesis techniques used to correct de- formities of lower limbs.8,9 However, the series reported methodolo- gical principles and did not look into risk factors for recurrence. Several publications reported possibilities with MRI to study bone condition in rickets-like diseases and osteomalacia.18 The previous work of Shevtsov et al., shown that MRI plays a substantial role in identifying physeal changes to be considered for a choice of treatment technique.20
Conclusion
A review of radiomorphological manifestations of lower limb long bones in patients with vitamin D-resistant rickets before and after de- formity correction showed that recurrent deformity can develop due to
progression of the disease with irregular formation of osteoid zones in the medial and lateral or lateral and posterior metaepiphysis, in- sufficient mineralization of the regenerate bone with an overall de- crease in the bone density, and formation of Looser’s zones, and in- crease in osteoid area of more than 50% of epiphyseal cross section.
Declarations of interest
None.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Holick MF. Resurrection of vitamin D deficiency and rickets.J Clin Invest.
2006;116(8):2062–2072.
- Thacher TD, Fischer PR, Strand MA, Pettifor JM. Nutritional rickets around the world: causes and future directions.Ann Trop Paediatr.2006;26(1):1–6.
- Abrams SA. In utero physiology: role in nutrient delivery and fetal development for calcium, phosphorus, and vitamin D–.Am J Clin Nutr.2007;85(2) 604S-7S.
- Feng JQ, Ward LM, Liu S, et al. Loss of DMP1 causes rickets and osteomalacia and identifies a role for osteocytes in mineral metabolism.Nat Genet.2006;38(11):1310.
- Ilizarov GA.Transosseous Osteosynthesis.Berlin, Heidelberg: Springer; 1992.
- Paley D.Principles of Deformity Correction.Berlin: Springer-Verlag; 2002.
- Sklyar K, Grebenyuk L. Pediatric operative treatment of post-rickets deformity of lower limb in children and adolescents and structural functional manifestations of femoral and tibial muscles (In Russian).Geniy ortopedii.2001:52–54.
- Kocaoglu M, Bilen FE, Sen C, Eralp L, Balci HI. Combined technique for the correction of lower-limb deformities resulting from metabolic bone disease.Bone Joint J. 2011;93(1):52–56.
- Petje G, Meizer R, Radler C, Aigner N, Grill F. Deformity correction in children with hereditary hypophosphatemic rickets.Clin Orthop Relat Res.2008;466(12):3078.
- Popkov D, Popkov A, Haumont T, Journeau P, Lascombes P. Flexible intramedullary nail use in limb lengthening.J Pediatr Orthop.2010;30(8):910–918.
- Song HR, Raju SV, Kumar S, et al. Deformity correction by externalfixation and/or intramedullary nailing in hypophosphatemic rickets.Acta Orthop. 2006;77(2):307–314.
- Subburaj K, Ravi B, Agarwal M. Computer-aided methods for assessing lower limb deformities in orthopaedic surgery planning.Comput Med Imag Graph. 2010;34(4):277–288.
- Shevtsov V, VolchkovaО. Age-related specific features of pediatric treatment of post- rickets and vitamin D-resistant rickets with the Ilizarov method (In Russian).Geniy Ortopedii.2008:51–54.
- Maltsev S, Arkhipova N. Genetically determined disorders of phosphatus metabolism in children and ways of their correction (In Russian).Kazansky Meditsinsky J. 2004:374–376.
- Popkov D. Application of intramedullary wires for limb lengthening (In Russian).
Vestnik travmatologii i ortopedii imeni.2005:65–69.
- Perwad F, Azam N, Zhang MY, Yamashita T, Tenenhouse HS, Portale AA. Dietary and serum phosphorus regulatefibroblast growth factor 23 expression and 1, 25-dihy- droxyvitamin D metabolism in mice.Endocrinology.2005;146(12):5358–5364.
- Diachkova G, Ryazanova E. Looser’s zones in patients with D-resistant rickets (In Russian).Travmatologiya i ortopediya Rossii.2009:74–79.
- Wehrli FW, Leonard MB, Saha PK, Gomberg BR. Quantitative high-resolution mag- netic resonance imaging reveals structural implications of renal osteodystrophy on trabecular and cortical bone.J Magn Reson Imaging.2004;20(1):83–89.
- Marie PJ, Glorieux FH. Relation between hypomineralized periosteocytic lesions and bone mineralization in vitamin D-resistant rickets.Calcif Tissue Int. 1983;35(1):443–448.
- Shevtsov V, Diachkova G, RyazanovaЕ. MRI, CT-semiotics of vitamin D-resistant rickets (In Russian).Vestnik Travmatologii i Ortopedii imeni.2009:43–47.