Technique for correction of combined burn scar deformity of foot

Hits: 238
TECHNIQUE FOR CORRECTION OF COMBINED BURN SCAR DEFORMITY OF FOOT
Case from practice
Running title: CORRECTION OF COMBINED BURN SCAR DEFORMITY
Кonstantin Novikov1,2, Michail Korostelev 3, Mohammad Reza Effatparvar4 , Natalia Shikhaleva1, Oleg Klimov1,
1Federal State Budgetary Institution Scientific Research Center named after academician G.A. Ilizarov »Ministry of Health of Russia, Kurgan.
2Federal State Budgetary Educational Institution of Higher Education «Tyumen State Medical University» of the Ministry of Healthcare of the Russian Federation, Tyumen,
3LLC «SМ-Clinik», Moscow
4Department of Anatomy, Biomedical science Group, university of Quebec , Quebec, Canada
*Corresponding author: К.I. Novikov
6, ul. М.Ulyanovoy, Kurgan 640014, Russia
Tel. (3522) 45-47-47, fax (3522) 45-40-60, 45-45-05
e-mail: office@ilizarov.ru, website: www.ilizarov.ru
Abstract
The post-burn deformity is a mixed plastic and orthopedic problem that impairs limb function and needs complex treatment. This essay reports a novel surgical treatment procedure performed for a patient with combined burn scar deformity of the dorsum of the feet and toes.
The surgical intervention included excision of coarse scars on the dorsal aspects of toes and both feet, autologous full-thickness skin grafting of cutaneous defects, and bilateral treatment of the subluxated metatarsophalangeal joints (MTPJ) using Ilizarov external fixation. Finally, deform toes were corrected, and the old scars were removed and replaced with new skin layers.
Keywords: Ilizarov Technique, Foot Deformities, scar, burns
Introduction:
The postburn foot deformities are the severe complication of thermal injury and are specified by their topographic location, the severity of the burn wound, and related scars. These factors play a crucial role in causing flexion and adduction contractures of the entire foot, flexion and extension contractures of toes, shortening of the Achilles tendon, and plantar aponeurosis. Among all postburn deformities, foot deformities make up 5-7% in adults and 10% in children. In addition, the dorsum of the foot is the most common involved area of the cases [1, 2], and accord as the results of cutaneous injury followed by scarring in conjunction with atherogenic dysfunction and the secondary involvement of underlying tissue into the scarring and the changes in the ligamentous, articular structures [3]. Scars that develop on the dorsum of the foot can result in hyperkeratosis or ulceration, adhesion of the skin to underlying tissues [2, 3], and lead to numerous difficulties such as limited plantar flexion, subluxation, digital joints dislocation, reducing the functional capacity of the segment, major cosmetic problems, and inability to wear regular footwear which highly impaired quality of life [4].
The available Surgical approaches include complete scar resection, skin grafts, local flaps, and free flaps avoid most of the mentioned difficulties. However, skin grafts and local flaps provide limited soft tissue coverage, which for the patients who have a shortage of donor tissue availability makes reconstruction surgery difficult in many cases and inapplicable for them. [5-8]. In our opinion, applying the Ilizarov deformity correction technique combined with plastic surgeries is the method of choice for such cases.
Case Report:
clinical observation
Operative interventions were performed on a 9-years-old patient who sustained boiling water burns a year before admission. She used natural home remedies for five months. The wounds healed with coarse scars, and the patient developed a severe burn scar deformity of the feet and disturbed gait.
Physical examination of the patient revealed coarse hypertrophic scars on the dorsum of the feet and the lateral surface of the tibiae. The scars were moderately painful at palpation. Evident bilateral desmogenic extension contracture of the third, fourth, and fifth toes in MTPJs was clinically observed in conjunction with flexion contracture of toes in interphalangeal joints. The range of motion in MTPJs was 10-15°. Radiological findings complied with the clinical presentation.

Fig 1. Photography of the feet before surgery

Fig 2. Radiography of the feet before surgery
operation
plastic:
The operation procedure started with plastic surgery. First, the scars were excised on the dorsum of the left foot at the base of the toes. Then, to repair the cutaneous defect, the opposing cut-off triangular flaps were applied and stitched via interrupted Donati stitches; Prolen 5.0 sutures were also employed to the skin. Meanwhile, maximum attempts were made to bring the toes to flexion but failed due to rigid MTPJs. Next, U-shaped flaps with the base to the plantum were cut off at the 2nd, 3d, and fourth interdigital web spaces and fixed at the dorsum of the foot at the level of MTPJs. Afterward, Full-thickness skin was harvested from the right-side groin area to cover the defect of the foot. The donor wound in the right iliac area was sutured layer after layer with interrupted Donati, Vicrul 4.0, and Prolen 5.0. Later, the graft was treated with the Krasovitov technique and placed at the cutaneous defect site. An aseptic dressing with atraumatic mesh gauze was also applied to the wound.
Ilizarov:
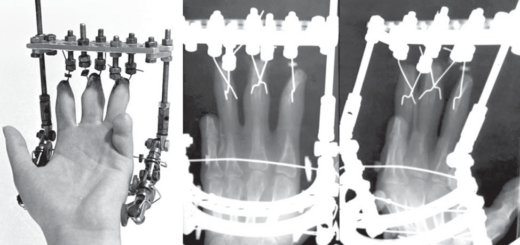
When the soft tissue procedure was accomplished, two opposing Kirschner wires with stoppers were placed in metatarsals bones in the horizontal plane. The wires were fixed to two frames on the plantar aspect of the foot and the frames connected with rods. Then, four distraction rods with hinges were attached to the distal support. After that, new 1 mm wires were inserted into the medial phalanx of the 2nd, 3d, 4th, and fifth toes, U-shaped and fixed to the rod connected with the frames. Finally, acute distraction was performed using the rods to maintain normal toes position. overall operating time was 90 minutes.
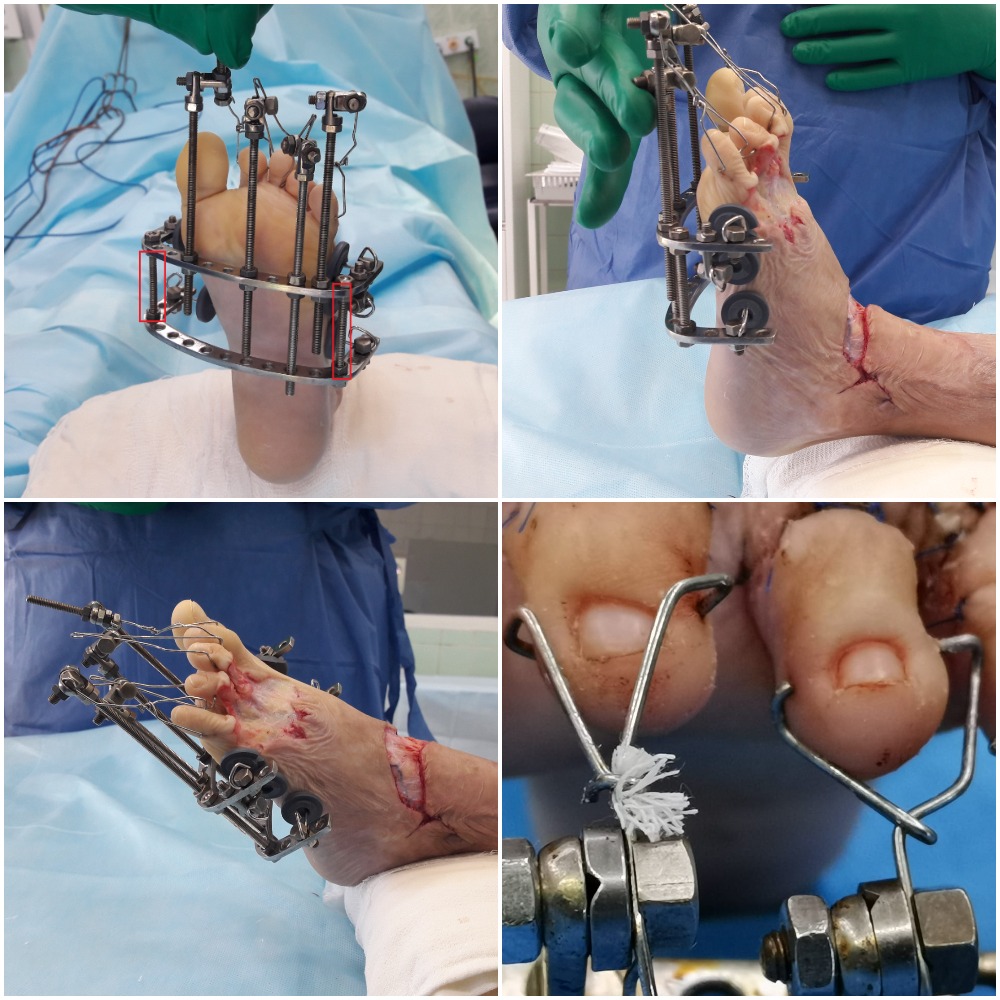
Fig 3. Intraoperative photography of fixator design.
Follow up
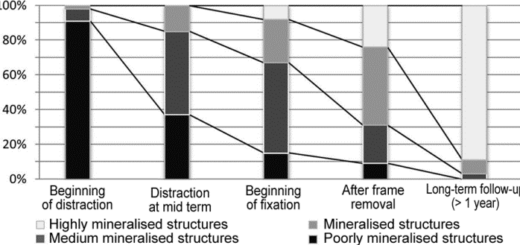
The day after the operation, gradual traction was provided for ten days to stretch and reduce subluxations in the 3d, 4th, and 5th MTPJs and bring toes to flexion.
The surgery was performed consecutively on both feet, first on the left side, and then a similar procedure was produced on the right side.
Full-thickness skin graft appeared to stretch easily and pain-free at toe traction getting the toes to flex. The toes were shown to get flexed, and the frame was transferred to the fixation mode for 21 days to allow full integration of autologous skin graft into the wound bed and was taken off simultaneously with suture removal.
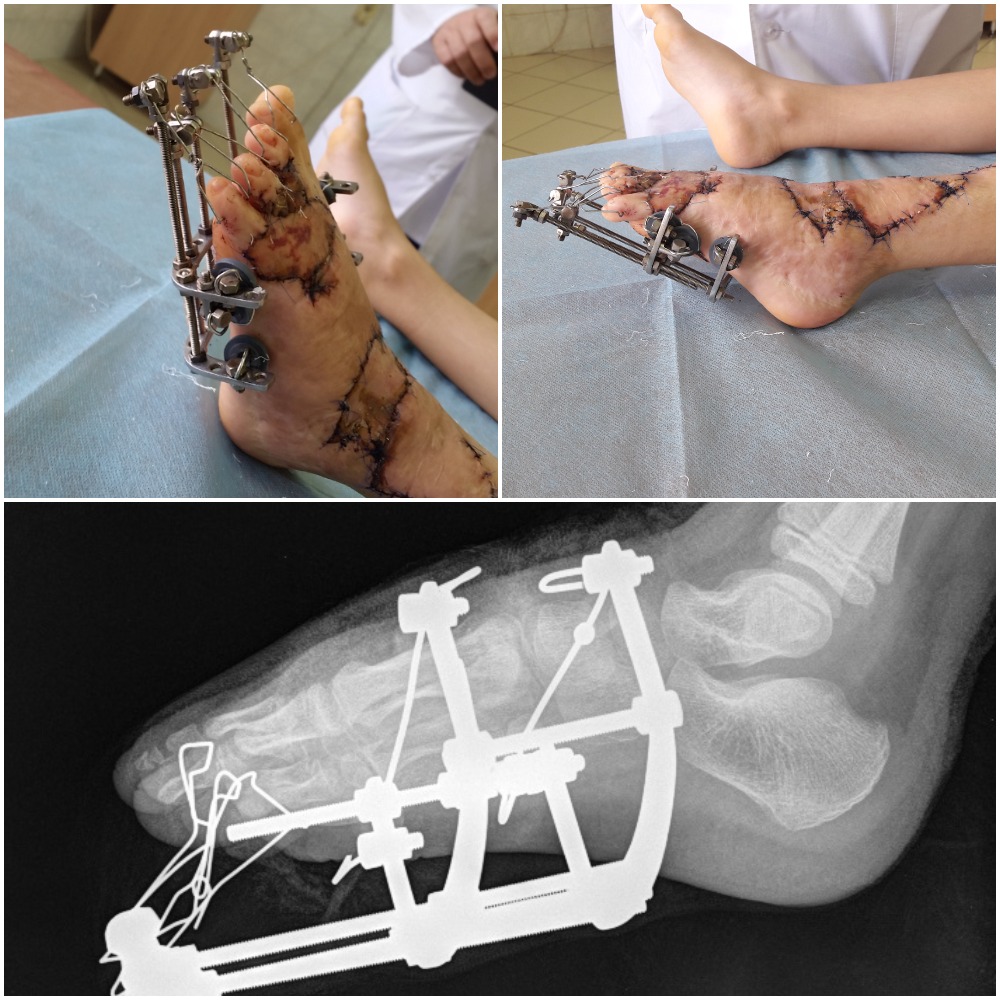
Fig 4. Post-operative photographic
The patient received antibiotics, medications to improve microcirculation, and rheological blood properties. No recurrence was observed at a 2-year follow-up with good function of both feet ensured.

Fig 5. The last outcome of correction

Fig 6. Finger function (flexion), the last outcome of correction
Discussion:
The above clinical study showed a severe burn foot deformity could be treated within one surgical session using combined skin plasty and the Ilizarov external fixation addressing subluxated toes, syndactyly, scars on the dorsum of the foot.
This technique provides observing the retention of grafted tissues, changing dressings, and patient mobility. Moreover, it was comfortable enough for the patient due to minimum forces developed by the frame and aimed to approach the particular component of the contracture.
The so-called lyre and wire traction or threaded soft tissue suture fixing toes to the plantar surface of the foot were traditionally used by surgeons to extend and hold the toes in the realigned position. The method was often associated with bedsores developing in the neighboring toes due to pressure from the needle spill or cutting through the soft tissues.
However, further improvement of the technique is needed to include classification, the algorithm of examinations, and selection of the treatment strategy depending on the individual characterization of anatomical and functional impairment of the foot. So, it would allow a more comprehensive application of the technique at different levels of the health care system.
Funding:
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflicts of Interest Statement:
The Authors declare that there is no conflict of interest.
References:
- Chang JB, Kung TA, Levi B, Irwin T, Kadakia A, Cederna PS (2014): Surgical management of burn flexion and extension contractures of the toes – J Burn Care Res, 35(1), 93–101.
- Heimburger RA, Marten E, Larson DL, Abston S, Lewis SR (1973): Burned feet in children: acute and reconstructive care – Am J Surg, 125(5), 575–579.
- Shakirov BM (2010): Evaluation of different surgical techniques used for correction of post-burn contracture of foot and ankle – Ann Burns Fire Disasters, 23(3)l, 137–143.
- Asuku ME, Ogirima MO (2007): The intravenous canula stylet as intraosseous fixator in the surgical correction of burn scar contractures of the foot in pediatric patients – Burns, 33(3), 378–381.
- Angrigiani C (1994): Aesthetic microsurgical reconstruction of anterior neck burns deformities – Plast Reconstr Surg, 93(3), 507–518.
- Shakirov BM (2015): Surgical treatment of post burn bent contractures of the foot in children – Clin Res Foot Ankle, 3(1), 1000166. doi: 10.4172/2329-910X.1000166.
- Shakirov BM (2007): Foot postburn bent contracture deformities – Burns, 33(8), 1054–1058.
- Constantino JA, Rodriguez-Yuste JA, Quiles M. (2007): Severe post-burn hyperextension of metatarsophalangeal joints in a child with bilateral foot contracture – J Foot Ankle Surg, 46(1), 48–51.