Orthopaedic, psychological, social and philosophical aspects of achondroplasia patients treated with the Ilizarov method
Hits: 272
© Diachkova G.V., Aranovich A.M., Diachkov K.A., Klimov O.V., Novikov K.I., Sutyagin I.V.
Orthopaedic, psychological, social and philosophical aspects of achondroplasia patients treated with the Ilizarov method
G.V. Diachkova, A.M. Aranovich, K.A. Diachkov, O.V. Klimov, K.I. Novikov, I.V. Sutyagin
Russian Ilizarov Scientific Center for Restorative Traumatology and Orthopaedics, Kurgan, Russian Federation
Introduction Achondroplasia is the most common skeletal dysplasia with limb shortening that can be symptomatically be treated with the Ilizarov method developed in the 20th century. Achondroplasia patients were shown to have medical and surgical possibilities for height increase with indications being controversial, and psychological and social implications to be considered. Objective The purpose of the study was to review our own data and reported findings on possibilities, results and complications of Ilizarov treatment of achondroplasia patients. Material and methods Outcomes of 750 achondroplasia patients treated at the Kurgan Ilizarov Center between 1976 and 2017 were reviewed. The patients’age ranged from 4 to 23 years. Results Long-term outcomes were followed up in all the cases. Radiography was used to assess limb elongation at follow-ups and MRI, MSCT and US were optional. Ten-to-fifteen-year follow-ups showed persisted length gain, early osteoarthritis of the hip and knee joints due to baseline articular changes, completely restructured femur and tibia at the distraction site, normal anatomy and area of muscle cross-section, normal structure and thickness of tibial muscles. Social and psychological profile appeared to improve. We have data from the patients who underwent limb lengthening 30 years ago. Many of them are employed, have family and children. Conclusion The findings suggest that achondroplasia patients, a comparatively small group of short statured people, have good reasons to feel empowered, get social support, make parents happy and contribute to the success of the country. The Ilizarov method has turned the idea of height increase into an accomplishment for benefits of doctors and patients being an achievement of orthopaedic world to address orthopaedic, social, psychological and philosophical issues.
Keywords: achondroplasia, Ilizarov method, limb lengthening, psychology, social and philosophical aspects
INTRODUCTION
The condition of locomotor system known to orthopaedic surgeons, geneticists, radiologists, artists as achondroplasia is included in Chapter XVII “Congenital malformations, deformations and chromosomal abnormalities (Q00-Q99), section “Congenital malformations and deformations of the musculoskeletal system” (Q77.4), group “Osteochondrodysplasia with defects of growth of tubular bones and spine” of the International Classification of Diseases [1]. Patients with achondroplasia have genetic changes in the transmembrane domain of the fibroblast growth factor receptor (FGFR) 3 gene encoding FGFR3 mapped at the short arm of chromosome 4p locus
16.3 with mutations resulting in the substitution
of arginine for the glycine residue at position 380 (Gly380Arg) in polypeptide of FGFR3 [2–4] causing locomotion deficiency. The condition is characterized by impaired bone growth and formation of muscles that are longer compared to the bone, short tendon and longer belly [3, 5–8]. Pathological manifestations of achondroplasia include changes in skeleton, other
organs and tissues (obesity, abnormal head shape, frequent otitis media, conductive hearing loss, respiratory insufficiency, apparent lumbar lordosis, spinal stenosis, radiculopathy, flat base of the skull, decreased foramen magnum diameter, etc.), appearance [4, 9–11]. Those with typical clinical and radiological features of achondroplasia do not need molecular genetic testing to confirm the diagnosis. However, if there is uncertainty, identification of the gene by molecular genetic testing can be used to establish the diagnosis [4]. The pathological changes typical for achondroplasia patients contribute to stereotype and lifestyle but changes in appearance with associated disproportionate short stature and limbs are reported as a matter of urgent priority. A complex of pathological changes in locomotor system revealing in specific clinical and radiological features and aggravating with age makes social adjustment difficult. The method of transosseous distraction osteosynthesis developed with the guidance of Professor G.A.Ilizarov contributed enormously to the treatment of achondroplasia to allow the patients
![]() Diachkova G.V., Aranovich A.M., Diachkov K.A., Klimov O.V., Novikov K.I., Sutyagin I.V. Orthopaedic, psychological, social and philosophical aspects of achondroplasia patients treated with the Ilizarov method. Genij Ortopedii. 2018. T. 24. No 4. pp. 465-473. DOI 10.18019/1028-4427-2018-24-4-465-473. (In Russian)
Diachkova G.V., Aranovich A.M., Diachkov K.A., Klimov O.V., Novikov K.I., Sutyagin I.V. Orthopaedic, psychological, social and philosophical aspects of achondroplasia patients treated with the Ilizarov method. Genij Ortopedii. 2018. T. 24. No 4. pp. 465-473. DOI 10.18019/1028-4427-2018-24-4-465-473. (In Russian)
benefit from changes in their orthopedic, social and psychological status [9, 12-15]. Treatment of achondroplasia patients using the Ilizarov method and different modified frames has been reported in multiple series of the recent decades showing controversial results and recommendations on therapies, meanwhile impossible, including genotype correlations, postnatal therapies for growth plates, potential postnatal FGFR3 therapies for children with achondroplasia [16–18].
Limb lengthening and deformity correction is the only orthopaedic option for achondroplasia patients, and Ali Al Kaissi et al. (2013) suggests that the role of the physician is fundamental in determining if the deformity is physiologic and requires no correction or in connection with an intrinsic bone disorder and should be addressed surgically [16]. Medical and surgical options are available to increase patient height, but indications are controversial, and treatment often consumes a large portion of the child’s life [10]. However, our experience has shown that all achondroplasia patients are predisposed to limb lengthening procedure even if they have no apparent deformities. Unique findings have been accumulated
at the Russian Ilizarov Scientific Center “Restorative Traumatology and Orthopaedics (RISC “RTO”) on treatment of achondroplasia patients by the numbers of cases done at the hospital and long-term follow- ups [9, 13, 19]. Clinical presentation and radiographs were reviewed by paediatric orthopaedic surgeons and radiologists specializing in musculoskeletal pathology. All patients operated on for achondroplasia were predisposed to limb lengthening procedure either by psychological or cosmetic reasons and had no contraindications to surgery. The investigation was performed in accordance with the ethical standards as laid down in the Declaration of Helsinki “Ethical principles for medical research involving human subjects”, amendments of 2013, and Order No. 266 of June 19, 2003 On Approval of Rules of Good Clinical Practice in the Russian Federation. The patients and legally authorized representatives gave informed consent for surgical procedure and publication of the findings without identification.
Objective The purpose of the study was to review
our own data and reported findings on possibilities, results and complications of Ilizarov treatment of achondroplasia patients.
MATERIAL AND METHODS
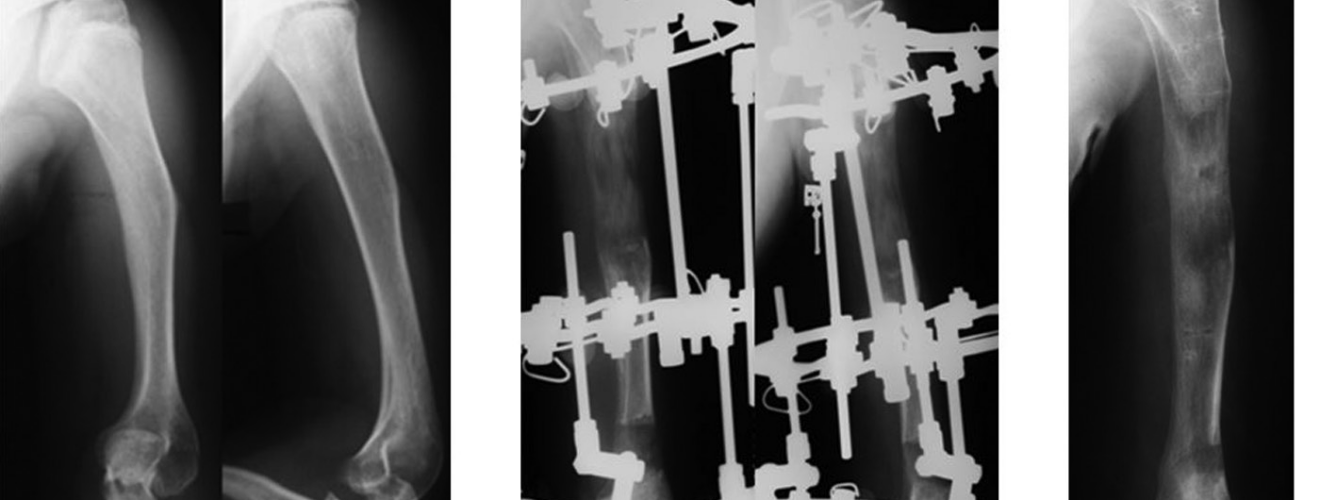
Outcomes of 750 achondroplasia patients treated at the RISC “RTO” between 1976 and 2017 were reviewed. The patients’age ranged from 4 to 23 years. There were 47 % of male and 53 % of female patients; 76 % aged from 6 to 14 years, 16 % from 15 to 17 years and 8 % older than 18 years. Low stature (< 4 % of average height for age), deformity of the knee, ankle, tibia of different extent were observed in all the patients at the first stage of treatment (Fig. 1). Treatment was commenced at the age of 6.0–
6.5 years producing consecutive mono- or bifocal tibial lengthening of 7.0–8.5 cm at the first stage followed by two-stage femoral and tibial lengthening of 10–12 cm using bifocal distraction osteosynthesis. Treatment was accomplished with humerus lengthening of 9.0–11.0 cm using bifocal distraction osteosynthesis (Fig. 2).
Operative technique. All surgeries were produced by qualified personnel with 10 years of experience in a specialized department and the highest qualification category. Surgical intervention was performed under
endotracheal anesthesia in all the cases using the Ilizarov techniques developed at the RISC “RTO” (Fig. 3).
Medical records, radiographs, multislice computed tomography, magnetic resonance imaging (MRI) were reviewed. Clinical presentation and radiographs were reviewed by paediatric orthopaedic surgeons and radiologists specializing in musculoskeletal pathology. All patients operated on for achondroplasia were predisposed to limb lengthening procedure either by psychological or cosmetic reasons and had no contraindications to surgery. The investigation was performed in accordance with the ethical standards as laid down in the Declaration of Helsinki “Ethical principles for medical research involving human subjects”, amendments of 2013, and Order No. 266 of June 19, 2003 On Approval of Rules of Good Clinical Practice in the Russian Federation. The patients and legally authorized representatives gave informed consent for surgical procedure and publication of the findings without identification.

Fig. 1 Radiographs of femurs and tibiae in achondroplasia patient aged (a) 14 years; (b) 11 years; (c) 8 years
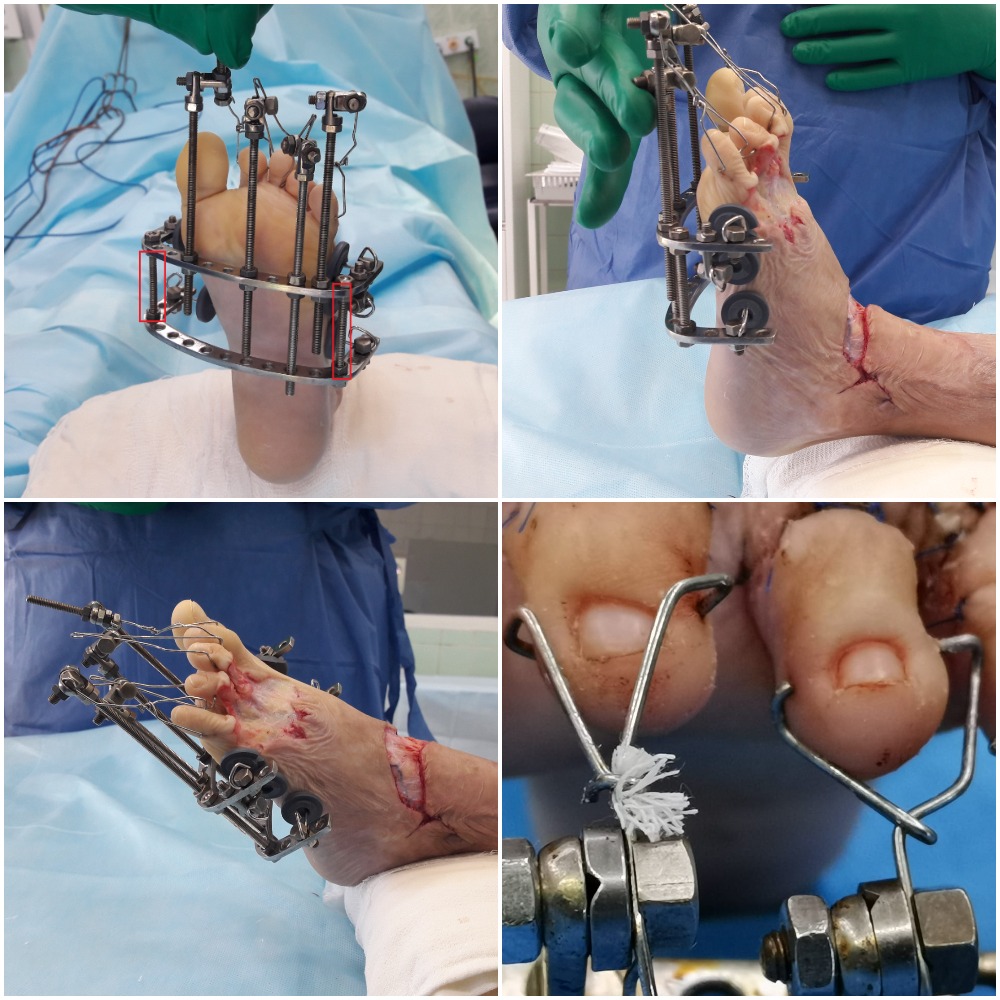
Fig. 2 Diagrams of tibial and femoral lengthening at different stages of treatment of achondroplasia patients showing (a) bifocal tibial lengthening; (b) cross lengthening of tibiae and femurs

Fig. 3 Diagrams of surgical interventions performed for achondroplasia patients at different stages of treatment: (a) tibial lengthening; (b) femoral lengthening; (c) humerus lengthening
RESULTS
Total length gain was 7.0–8.5 cm at the first stage and 17.0–18.0 cm at the second stage including two cross lengthening (left tibia and right femur, then right tibia and left femur, for instance) (Fig. 4).
75 % of the patients insisted on lengthening of humeri
with the length gain measuring 10.1 ± 1.5 сm (Fig. 5).
Long-term follow-ups were reviewed in all the cases
with ultimate observation period of 30 years. Condition
of the segment lengthened was examined clinically and radiography at follow-up visits; MRI, MSCT and US were used if needed. The patients were treated at several stages with an interval between them being dependent on a phase of treatment, the segment lengthened, quality of new bone, muscle and joint functioning and the beginning of the next stage of treatment and rehabilitation program were considered and discussed during follow-up visits. The treatment was normally complete with tibiae lengthened, cross lengthening of femurs and tibiae and humeri elongated. Twelve-to- eighteen-month follow-ups showed complete bone restructuring, formation of intramedullary canal and cortical bone with normal three-zonal pattern (Fig. 6).
The question of what happens to achondroplasia patients 10, 15, 20 years of limb lengthening was frequently discussed in the literature. Review of 10-to-15-year follow-up demonstrated the persisted length gain, early signs of knee and hip osteoarthritis due to baseline changes, complete bone restructuring at the sites of tibial and femoral lengthening, normal anatomy and area of muscle transverse sections, normal structure and thickness of tibial muscles and less thickness of subcutaneous fat tissue compared to preoperative value (Fig. 7).
We have data from the patients who underwent limb lengthening 30 years ago. Many of them are employed, have family and children.

Fig. 4 Radiographs of tibiae of achondroplasia patients showing (a) preoperative view, (b) lengthening accomplished; (c) lower limbs after cross lengthening of the right femur and left tibia; (d) lower limbs after the second cross lengthening
Fig. 5 Radiographs of humeri of achondroplasia patients showing (a) preoperative view; (b) the bone being elongated; (c) bone lengthening accomplished

Fig. 6 MSCT of tibia of achondroplasia patient at 14-month follow-up showing (a) MPR in coronal plane; axial scan of MSCT of tibiae at 16-month follow-up; (c) VRT; (d) MRI of tibiae at 18-month follow-up, T2WI, coronal plane

Fig. 7 CT scans of lower limbs of a 22-year-old female patient Kh. showing (a) lower limbs at 12-year follow-up; (b) axial view at the upper third of the femur (lengthening site); (c) ultrasound image of anterior tibial muscle and the long digital extensor tendon of both tibiae
DISCUSSION
The success of treatment of achondroplasia patients depends on many factors and is determined by high motivation of the patient, joint function, extent of spinal changes, tactics of surgical treatment, experience of the surgeon, possibilities with adequate rehabilitation, amount of limb length gained, patient’s growth following limb lengthening, appearance of normal proportions between torso and the limbs and the education received throughout the treatment. Joint function is of special concern with limb lengthening since it is found to be preoperatively specific and typical for achondroplasia patient. However, exercise therapy and physioprocedures can improve the scenario although early arthritis of the knee, hip and ankle joint is common for adult achondroplasia patients but the condition is not severe and requires no arthroplasty. Many orthopaedic, social and psychological aspects can be addressed during the
treatment of achondroplasia patients and there is a philosophical implication brought up by Prof. C.R.Michel in his article Philosophie de L’Orthopedie, 1998. Prior to treatment an achondroplasia person can put a question ‘Shall I become a taller dwarf or a person of a short height?’ [20]. This is not a simple question to answer because the Ilizarov method in contrast to other great achievements of the 20th century including arthroplasty, spine surgery and endoscopy bears a greater philosophical burden due to the duality (possibility and necessity):
1) philosophy of the inventor who discovers the possibility of human growth at any age; 2) whether there are indications to the treatment of people with insufficient growth [20]. Therefore, the goal of the physician, patient and the parents is to make the proper choice and put the possibilities of the method into operation to allow achondroplasia person be a
short individual with good perspectives of social and occupational adaptation. The perspective is more than good for the patients who start the treatment on time going through the stages of tibial lengthening, cross lengthening of femurs and tibiae as the second phase, humerus lengthening, who receive support from parents, are able to have a good rehabilitation program, make efforts to be a diligent student at school (classes available at the Ilizarov Center) and can receive higher education [21, 22]. Young female patients opt for a minor cosmetic procedure erasing last traces of achondroplasia and finding the place in the world. Doctors, engineers, mathematicians, people engaged in public activities are among our patients. There are nonprofit organizations of little people who underwent Ilizarov limb lengthening that provide support and information to people of short stature and their families. The Russian Association of Parents of Children with Achondroplasia has been established in Russia and there are similar organizations set up in different countries including those that focus on genetics evaluation of children, for instance, the American Academy of Pediatrics Committee on Genetics [4]. Surgical interventions produced for achondroplasia patients can be considered as curative (varus deformity) and prophylactic or performed for cosmetic reasons. “Prophylactic operative procedures if can be justified should entail neither errors nor complications” [20]. We all accept ethical requirements of our profession and are to be honest with ourselves and be ensured we can provide the patients with the best chances of recovery. This is the only condition to take upon oneself and survive failure: ‘without failure, no ethics’ (Simone de Beauvoir, cited by Michel C.R., 1998) [20]. Who can ensure the safety of lengthening of an absolutely healthy limb? Long-term outcomes showed that patients reported substantial cosmetic effect, improved gait and self- esteem. Complications observed during treatment and at a short term due to specific anatomy of the skeleton and other parts of the body in achondroplasia patients, an extensive period of treatment, a greater length gain included regenerate deformity and fracture, joint contracture and neurological problems. The complication rate ranged from 11 to 20 % and were addressed before the treatment was accomplished or at an early postoperative period [23– 26]. Different rates and types of complications are reported in the series of foreign authors. H. Kitoh, K. Mishima, 2014, reported 11 regenerate fractures in eight out of 24 patients who underwent 70 segmental
limb lengthening [27]. I. Kadono, 2018, observed development of contractures of several joints in 6 patients following tibial lengthening that gradually resolved with dedicated physiotherapy [28]. As it was mentioned, surgical stage of treatment is a part of the problem that achondroplasia patients and the parents have to address. Psychological wellbeing is essential for many aspects of patients’ life. A lot of research has been conducted to assess psychological profiles of achondroplasia patients prior to and after treatment [19, 29, 30]. The greater part of the works has been produced at the Ilizarov Center and demonstrated changes occurred in psychological wellbeing, social adjustments and routine activities after limb lengthening. Patients reported appearance related concerns at school before treatment. Everyday activities such as shopping, using public transport, and simple bathroom and toilet hygiene were difficult for people with short stature and disproportionately short limbs. Teenagers and elder patients pursued their dreams through college and career [15, 19, 29]. A nationwide survey made by foreign specialists to assess psychosocial profiles of children with achondroplasia before treatment showed that they experienced more short stature-related stressors with no evidence of any psychosocial maladaptaion [31].
A.C. Rohenkohl et al., 2015; J. Quitmann et al., 2014, focused on behavioral and psychological problems, assimilation of people of short stature into community with the need to provide care and support to them [32–34]. Surveys collected by
S.E. Gollust et al., 2003 from individuals affected with achondroplasia and unaffected first-degree relatives in the United States showed that the affected people had lower annual income, less education and were less likely to be married than unaffected relatives [35]. T.L. Trotter, J.G. Hall, 2005 made a clinical report for pediatricians and families in caring for children with achondroplasia from the prenatal visit through childhood and adolescence to early adulthood discussing psychosocial implications [4]. Literature review and our own findings have shown that treatment of achondroplasia patients cannot be considered as solely an orthopaedic issue since evident psychosocial implications and philosophical aspects involve the enhanced teamwork of orthopaedic surgeon, psychologist, social services and the community into the treatment process with one goal in mind: to allow the patient benefit from surgical intervention being consistent with an integral part of the Ilizarov philosophy [36, 37, 38, 39].
CONCLUSION
The findings of the study indicate that achondroplasia patients need both orthopaedic treatment and psychological and social support. A comparatively small group of short statured people have good reasons to feel empowered, get social support, make parents happy and contribute to the success of the country. Many years have passed since the patients diagnosed with achondroplasia had a chance to become an individual whose potentialities were not limited by short stature thanks to the brave genius of Professor G.A.Ilizarov. As noted by Clavel Bernard Charles, ‘an idea can be in the air for
months, years, sometimes for centuries and pass from hand to hand like a rugby ball until a man of genius would implement it in such an impressive, significant, unforgettable manner like a rugby player would squeeze the ball at an attempt. It is only then that the idea becomes a part of the public domain, and the discovery being evident’ [cited by Michel C.R., 1998] [20]. It can be equally relevant to the method of Ilizarov who has turned the idea of height increase into an accomplishment for benefits of doctors and patients being an achievement of orthopaedic world to address orthopaedic, social, psychological and philosophical issues.













